How Much Lead is Detrimental to Health?
I just recently became aware of the effort to bring the AtlasBX automotive battery plant to Clarksville. This plant will release a non-insignificant amount of lead into our community. Is this OK?
In the world of medicine we believe that we should never do anything to a patient without informed consent – this means the patient is aware, educated, and able to comprehend the potential benefits and risks of the intervention, whatever that may be. This is my attempt to help the process of informed consent regarding our community bringing another lead-releasing industry into our area.
The Economic Development board of Clarksville is an amazing group of individuals that do an amazing job for Clarksville from an economic standpoint by bringing jobs to the community, and for that I commend them. They as a group are a real asset to this community. The economic benefit of a new lead-battery plant (and the Zinc Plant – which is a larger polluter by volume at present) is easy to see from measurements of jobs, dollars, and people moving to Clarksville. They, of course, are not experts in the effects of toxic substances on the health of a population so they depend upon the transparency of industry and the cooperation and excellence of governmental oversight organizations.
The health risks of toxicity to our community are much harder to see, to understand, and to take seriously in a time and age when we are distracted at every moment by some email, call, notification, or 24-hour news cycle created crisis. Taking toxicity seriously requires us to think about our health, the health of our children, grandchildren and great-grandchildren, the health of our land, and acting with wisdom rather than reflex. The risks of lead are very real, at very low doses, for a very long time.
Just thinking about toxins is repulsive to most folks, because we want to believe if we just put our head in the sand everything will be OK. We want to think the governmental agencies that are there to protect us from the unseen dangers of toxins are doing their job and are being appropriately proactive, but in the end it is up to us to become informed, and to give consent, or not.
Here are some facts:
Lead is highly toxic, at very low doses, and when it comes into the body or the soil it is not easily or quickly removed. Lifetime lead accumulates in the body. Once the body or soil is polluted, it is difficult and resource-intensive to remove in comparison with avoidance of exposure in the first place. AVOIDANCE is key.
We have known since 2004 that there is NO SAFE level of lead for children – even the smallest measurable amounts decrease IQ and increase ADHD, violent crime, health care costs and decrease lifetime earnings. Blood lead levels are related to violence levels in communities and prisons. Elevated lead in members of our community effect the whole community in subtle but important ways.
In adults, lead impacts erectile function, fertility, sperm counts and miscarriage rates. Neurological effects include peripheral neuropathy, fatigue/irritability, impaired concentration, hearing loss, seizures, encephalopathy, and dementia. Lead can cause nausea, heartburn, constipation, anemia, constipation, kidney disease, high blood pressure, heart disease, muscle pains, and joint aches. This is what an EPA teaching sheet says about lead in the body – https://www.epa.gov/sites/production/files/2017-02/documents/wkrch2_stu_eng.pdf.
In 2018, it was published that even low levels of lead in adults (these would be levels considered in the “normal reference range” on a blood test) increase the risk of all-cause death, death from coronary artery disease, and death from ischemic heart disease. A 2018 study published in The Lancet Public Health suggests that of the 2.3 million deaths every year in the US, about 400,000 are attributable to lead exposure, of which 250,000 are from cardiovascular disease.1
What about kidney disease? In a study published in the Journal of the American Society of nephrology, 121 patients who had chronic renal insufficiency, a normal body lead burden (BLB), and no history of exposure to lead were observed prospectively for 48 months. What were the results? It turns out that even levels of Blood Lead and Body Lead Burden that are so low they are considered in the “normal range” are one of the most powerful predictors of decline in people diagnosed with kidney disease. Yep. “Normal” levels found in the population are still detrimental to the kidneys.
If lead is such a problem, we would expect its removal to decrease disease burden in children – has this been found? Yes.
First of all, the removal of lead from gasoline, paints, pipes, and household items has been a big win for health. Lead levels in young people are much lower than they used to be historically, and this has been associated with an increase in IQ, decrease in violent crime, decrease in special education needs, and higher earnings. But according to a study by the Pew Charitable Trust, the current excess cost of children living in homes with lead paint are estimated to be $192 to $270 billion over those children’s lifetimes due to increased need for health care, IQ loss, increased special education needs, lower earnings, behavior problems and crime. For every dollar invested in remediating lead paint where children are exposed there is an estimated $17 gain for society.
How about in adults – does the removal of lead associate with improved health outcomes? Yes.
In a large NIH-sponsored randomised controlled trial of patients who had a myocardial infarction, chelation with IV-EDTA, which removes lead, and multivitamin therapy led to an 18% reduction in cardiovascular events; patients with diabetes in the trial had a 34% reduction in cardiovascular events.15
Of note, the study was designed to show if IV-EDTA was a helpful component of a comprehensive cardiac disease care program, and did show that, however the study designers did not even measure before and after lead levels. The cost to do so is not substantial in comparison with the rest of the study costs, but instead measuring lead was considered too “political” to attempt as part of the study. Read on and you may understand why. Regardless IV-EDTA showed benefit in this study.
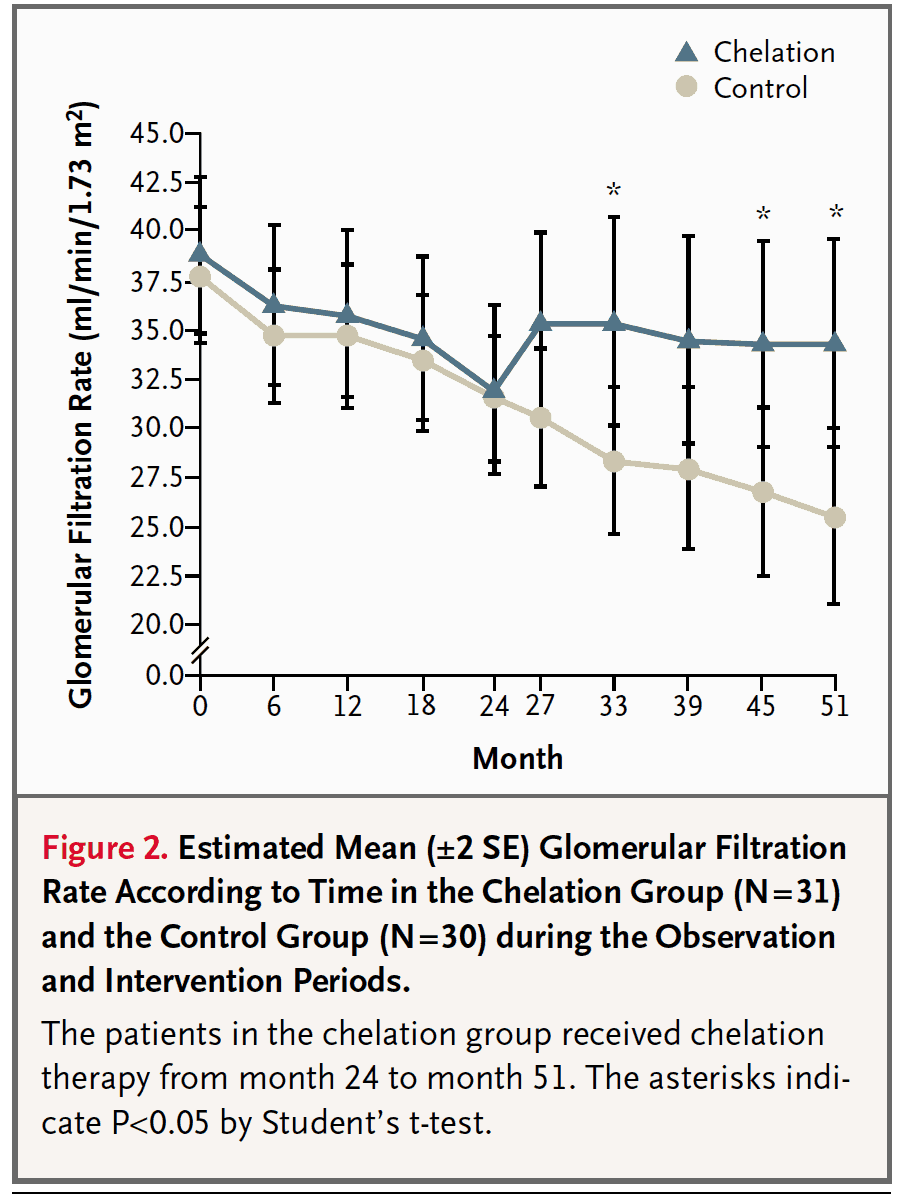
Does EDTA IV Chelation help to treat this low-level-lead-induced renal toxicity? The following study says “Yes”.
In a remarkable study published in the New England Journal of Medicine (not too shabby of a journal), 64 patients were followed for over 4 years. First, they split the group up into two groups and just monitored their kidney function for 2 years and saw that both groups had the same slow almost-thought inevitable decline of kidney disease. Then, half the group got EDTA-chelation therapy and their kidney function decline halted and did not progress over the 27 months of the study (the blue line below), while the control group (the tan line below) continued their slide towards increased death and dialysis. 16 Nothing says it like this picture. Which curve would you choose to be part of?
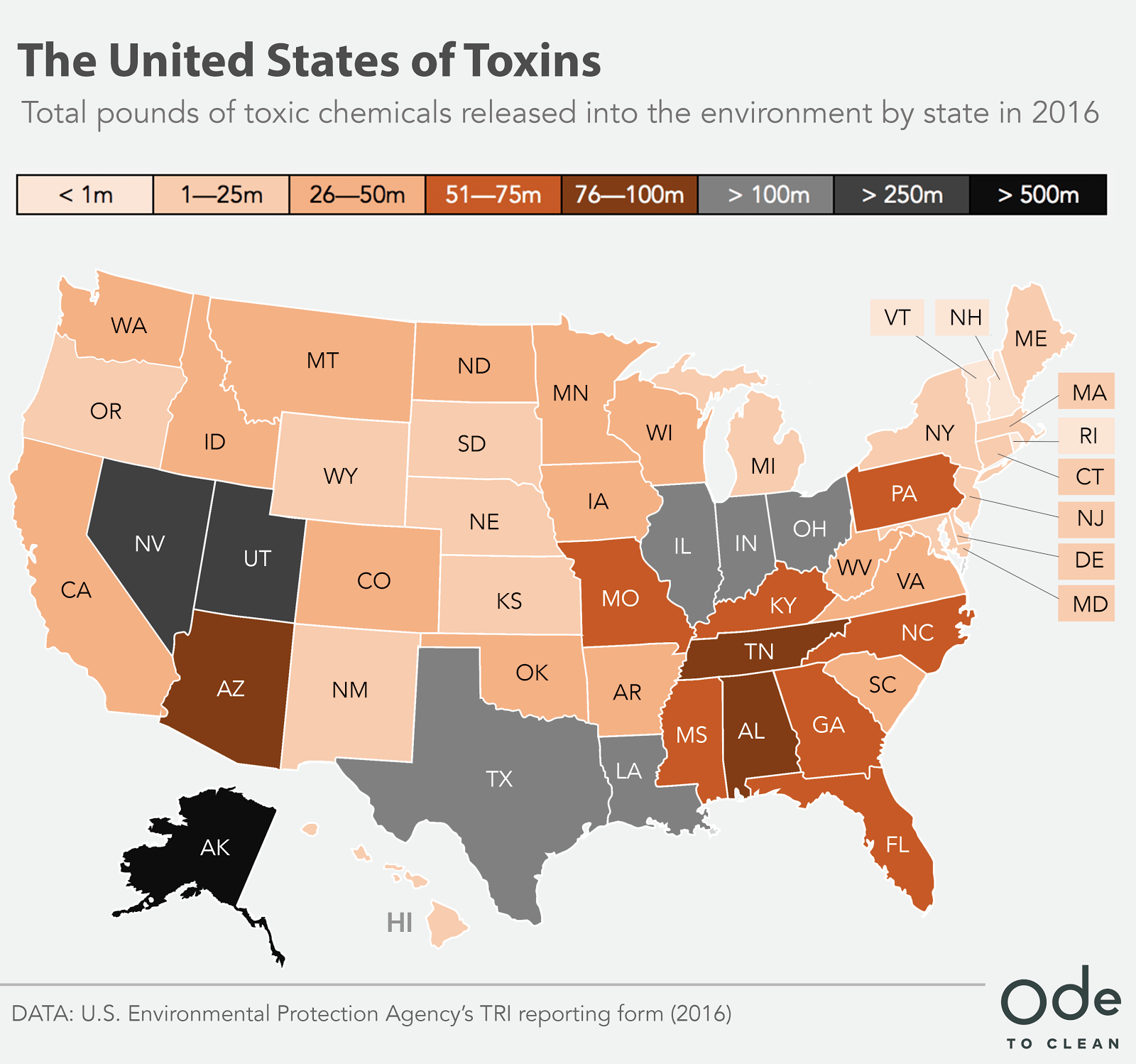
So, is one more source of lead in the area a big problem? Clarksville already rates as the 24th most toxic city in the US – right behind New Johnsonville, TN at 23! The cumulative load of toxins we are exposed to matters more than which company or food or water supply caused the exposure. Every little bit counts.
The following graphics are from OdetoClean. Why is Clarksville already at #24 most toxic city in the nation?
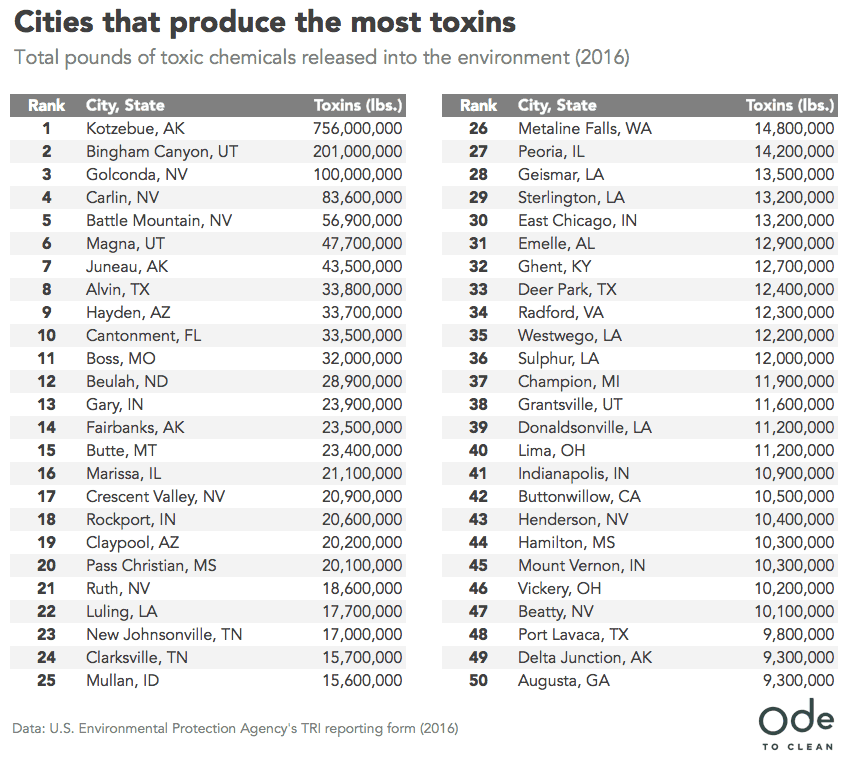
If you want to see how much Cadmium or Lead the Nyrstar Zinc plant releases, go to this site for a report on the numbers.
After reading this, like hell I am ever eating a fish from the Cumberland or Lake Barkley again. Cadmium has a near 40 year half-life – that means once it is in your body it takes 40 years for half of it to be removed (without the help of chelation therapy). Cadmium is a clear carcinogen – and effects are measurable at low doses. Lead is about a 20-30 yr half-life because it complexes in the bones. This is a presentation by the EPA discussing what a “release” is and your right to know as a citizen of the United States.
With this level of importance in human health and risk of exposure we all want simpler answers. Yet, the study of toxic metals and the relationship to health and medical care is complex for many reasons.
- It is reasonable to imagine that some individuals within industry do not want to believe it is a problem – can you imagine the workers’ compensation claims if there were more awareness or larger studies of this topic? Lots of rea$on$ for not wanting more information can be imagined – and since big businesses are often large contributors to political campaigns, few elected officials are really excited about championing this cause.
- Different forms of metals, and different routes of exposure have different levels of toxicity to the body at different ages – sometimes the exposure to a toxin greatly precedes the time period where the effect is seen.
- There is no big money driving research. Frankly, what we need is a new pharmaceutical company that develops a new chelator that they can make a bunch of money from to get the research we need – but until then we have smaller and shorter studies than we want.
- Measuring Toxic metals is tricky – blood lead levels are standard, but assessing the total body burden via more involved methods (like a chelation challenge test) seems to correlate more strongly with known health effects. Other metals require different testing methods yet.
- Blood tests with results within the “Normal Reference Ranges” for lead – and other toxic substances – are not representative of the best state of health possible. I think most can agree that ideal would be zero. “Normal” results such as these have been implicated in increased heart disease, kidney disease progression, and lower childhood IQ – and that is certainly not the normal I desire for my community.
- Toxins do not exist in isolation, research supports the combination of 2 toxins is not an additive effect, but a multiplicative effect. Effects of toxins such as alcohol, tobacco tar, pesticides, etc, contribute in their own ways which complicates the capacity to accurately ascribe effect to a single toxin.
- Each person has unique genetics and different capacities to detoxify and different levels of susceptibility to various toxic substances.
- Many other factors than toxic metals determine the health and well-being of an individual. Many of these factors – such as diet, activity, sleep, hormones, stress, relationships, infections, allergens, non-metal toxins and inflammation should be dealt with first before blaming toxic metals as the cause of all ills – yet toxic metals may not be ignored.
- Taking toxins out of the body via IV chelation works, but it is time consuming, and neither the major insurance companies nor Medicare are currently paying to remove toxic metals in non-acute poisoning scenarios. Even individuals with heart disease or renal disease that likely have lead as a contributor to the process almost always have to pay out of pocket for chelation therapy.
- The medical community itself is divided on when to treat whom and for what and with what. Much data exists and many strong differing opinions exist from doctors on this topic. In the past “chelation therapy” has had rabid evangelists and opponents – both of whom I feel have failed to appreciate the complexity of the situation, and thankfully both extreme camps seem to be diminishing in favor of a more moderate scientific curiosity and practice.
- Because of the complexities of diagnosis, treatment and billing, few health care facilities offer investigations beyond basic blood testing using reference standards where “normal” is still associated with increased risk of disease, or offer chelation therapy for non-acute poisoning even as the evidence base has grown (but is in no way universally agreed upon) for its utility in selected patients.
- Detox as a topic has become toxic. One quick search of the internet can return hundreds of self-proclaimed non-licensed experts as bloggers looking for just a quick click to drive advertising revenue, their own ego, or to sell some overly hyped process or product to “detox.” Detoxification is a real thing, but the way it is all-too-often sold in the blogosphere increases the cynicism of intelligent people on the topic.
So yes, everything about lead and its relationship to health is complex in the details, but very simple in the conclusion. Lead is bad for health. Less exposure is better for health. “Acceptable” levels of release and exposure are only acceptable in my opinion if they are not in the vicinity of my family, patients, and neighbors.
I hope Clarksville and our amazing Economic Development Board continues to concentrate on bringing clean industry to town, and allowing industry that has a higher chance of impairing the health and well being of our community to find another home.
Choosing wisely is the difference between being a community that leads and one that is led.
David H. Haase, MD
Founder, MaxWell Clinic, Clarksville & Nashville
CMO, MaxWell Biosciences
Faculty, Institute for Functional Medicine
________________
For further reading, these are excerpts from a great article on the health effects of lead posted on the website of the Institute for Functional Medicine. Used with permission – and this is the original link… https://www.ifm.org/news-insights/understanding-lead-toxicity/
A 2018 study published in The Lancet Public Health suggests that of the 2.3 million deaths every year in the US, about 400,000 are attributable to lead exposure, of which 250,000 are from cardiovascular disease.15
This estimate is about 10x larger than previous approximations;1 the Global Burden of Disease study estimated that 558,000 deaths were attributed to lead in 2015.2
Lead is one of many recognized risk factors for cardiovascular disease, and Lanphear et al were the first to test whether the relation with cardiovascular disease mortality was evident in a population with concentrations of lead in blood below 5 g/dL.1 Previously, amounts of lead in blood lower than 10 g/dL were associated with cardiovascular disease mortality.
Results from Lanphear et al suggest that low-level lead exposure is an important risk factor for death in the US, particularly for cardiovascular disease deaths.1
Lead is one of the most widely used metals in the world,3 and although it is toxic, it has been incorporated into different products including paints, cosmetics, fuel, etc. for its unique properties like low melting point and resistance to corrosion.4 However, lead persists in the environment and cannot be metabolized in the human body.3
It can enter the body via a variety of routes; particles from lead-based paint or housing renovation can adhere to food and be ingested, and industries that use lead in manufacturing can pollute the air and soil, exposing humans via the food chain.5 Lead can be absorbed by the intestine and through the skin, and almost 90% of it binds to erythrocyte proteins (albumin).4 Once inside the human body, lead may travel to different tissues and organs, including the liver and kidney, where it can exhibit oxidative damage on cells and tissues, and on cellular organelles by uncoupling the respiratory chain in mitochondria.4 DNA damage is a significant consequence of oxidative stress.3
A 2018 study provides the first published evidence that lead exposure results in DNA damage via promoting oxidative stress and the promoter methylation of DNA repair genes in human lymphoblastoid TK6 cells.3 There are limitations to this study. For example, it was carried out on only one human cell line, whereas the obtained results need to be verified in multiple human cell lines, and the role of DNA repair proteins in lead-induced genotoxicity is unclear and needs further elucidation. Taken together, however, the study results indicate that lead exposure decreased cell viability, induced oxidative stress-mediated DNA damage via the Nrf2-ARE signaling pathway, and decreased the expression of DNA repair genes.3
Lead has also been associated with peripheral arterial disease, electrocardiographic abnormalities, and left-ventricular hypertrophy.1 Due to the major route of excretion from the body, the kidneys are more vulnerable to lead; it promotes kidney damage via oxidative stress and lipid peroxidation.4 Lead has also been known to induce an inflammatory cascade in various tissues, causing respiratory, neurologic, digestive, cardiovascular, and urinary diseases.6
A population-based case-controlled study suggests that prenatal exposure to lead and cadmium, as reflected by their concentrations in placental tissues, may be associated with an increased risk for neonatal orofacial clefts.7 A number of studies suggest that lead exposure disproportionately affects children in lower-income neighborhoods, and even older children ages 5 to 12 years may be at risk of central nervous system effects.8
A 2018 study compared blood levels of older children from a historically contaminated urban neighborhood to those of demographically matched children from a nearby rural locale, and predicted significantly higher blood lead levels in the urban children.8
In 1979, Needleman et al suggested that lead exposure in children, at doses below those producing symptoms severe enough to be diagnosed clinically, appears to be associated with neuropsychological deficits.9 In 2004, a study published in Environmental Health Perspectives reviewed recent developments across the globe on the subject of low-level lead exposure and children’s cognitive development, and found that there is no safety margin at existing exposures.10 Despite seeing a reduction in lead exposure over time, Koller et al state, “it could be argued that current baseline blood levels continue to constitute a global public health risk.”10
A recent study suggests that the regular consumption of beverages in glazed, ceramic cups increases the chances of lead-related health risks.11 The chronic daily intake of lead by children and adults, respectively, consuming from new ceramic cups were 1.3–5× and 1.28–6× more than that from old ceramic cups. In both cases, intake values far exceeded the WHO reference dose of 0.0006 mg Pb/kg bw/day in children (<11 years) and 0.0013 mg Pb/kg bw/day in adults. According to the study, these levels of lead consumption in children might be predicted to be associated with a decrement in IQ by at least one point and associated with adverse effects in adults, especially women of childbearing age.11
Studies suggest that lead is a carcinogenic factor in animal models, and epidemiological studies have suggested the association of blood lead concentration and death rate due to cancer in a number of populations, including the US,12 South Korea,13 and Australia.14 In June 2018, the first study to demonstrate urinary lead concentration as an independent predictor of cancer mortality in the general population was published in Frontiers in Oncology.5
Using National Health and Nutrition Examination Survey 1999-2010 data and its Mortality Follow-Up study, Li et al found that “despite the marked decrease in environmental lead levels over the past three decades, lead exposure is still the significant determinant of cancer mortality in general population in US, and quantification of urinary lead may serve as a non-invasive approach to facilitate biomarker discovery and clinical translational research.”5
Portions of the above write-up is from The Institute for Functional Medicine, an organization of which I, David Haase, MD am on faculty. I have copied here with permission. This is the original link. https://www.ifm.org/news-insights/understanding-lead-toxicity/
References:
1. Lanphear BP, Rauch S, Auinger P, Allen RW, Hornung RW. Low-level lead exposure and mortality in US adults: a population-based cohort study. Lancet Public Health. 2018;(3)4:e177-184. doi:10.1016/S2468-2667(18)30025-2.
2. GBD 2015 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659-1724. doi:10.1016/S0140-6736(16)31679-8.
3. Liu X, Wu J, Shi W, Shi W, Liu H, Wu X. Lead induces genotoxicity via oxidative stress and promoter methylation of DNA repair genes in human lymphoblastoid TK6 cells. Med Sci Monit. 2018;24:4295-4304. doi:10.12659/MSM.908425.
4. Rana MN, Tangpong J, Rahman M. Toxicodynamics of lead, cadmium, mercury and arsenic-induced kidney toxicity and treatment strategy: a mini review. Toxicol Rep. 2018;5:704-713. doi:10.1016/j.toxrep.2018.05.012.
5. Li S, Wang J, Zhang B, et al. Urinary lead concentration is an independent predictor of cancer mortality in the U.S. general population. Front Oncol. 2018;8:242. doi:10.3389/fonc.2018.00242.
6. Boskabady M, Marefati N, Farkhondeh T, Shakeri F, Farshbaf A, Boskabady MH. The effect of environmental lead exposure on human health and the contribution of inflammatory mechanisms, a review. Environ Int. 2018;120:404-420. doi:10.1016/j.envint.2018.08.013.
7. Pi X, Qiao Y, Wei Y, et al. Concentrations of selected heavy metals in placental tissues and risk for neonatal orofacial clefts [published online July 24, 2018]. Environ Pollut. doi:10.1016/j.envpol.2018.07.112.
8. Alvarez J, Del Rio M, Mayorga T, Dominguez S, Flores-Montoya MG, Sobin C. A comparison of child blood lead levels in urban and rural children ages 5-12 years living in the border region of El Paso, Texas [published online July 28, 2018]. Arch Environ Contam Toxicol. doi:10.1007/s00244-018-0549-3.
9. Needleman HL, Gunnoe C, Leviton A, et al. Deficits in psychologic and classroom performance of children with elevated dentine lead levels. N Engl J Med. 1979;300(13):689-695. doi:10.1056/NEJM197903293001301.
10. Koller K, Brown T, Spurgeon A, Levy L. Recent developments in low-level lead exposure and intellectual impairment in children. Environ Health Perspect. 2004;112(9):987-994. doi:10.1289/ehp.6941.
11. Mandal PR, Das S. Leachable lead and cadmium in microwave-heated ceramic cups: possible health hazard to human [published online August 14, 2018]. Environ Sci Pollut Res Int. doi:10.1007/s11356-018-2944-8.
12. Cheung MR. Blood lead concentration correlates with all cause, all cancer and lung cancer mortality in adults: a population based study. Asian Pac J Cancer Prev. 2013;14(5):3105-3108. doi:10.7314/APJCP.2013.14.5.3105.
13. Kim MG, Ryoo JH, Chang SJ, et al. Blood lead levels and cause-specific mortality of inorganic lead-exposed workers in South Korea. PLoS One. 2015;10(10):e0140360. doi:10.1371/journal.pone.0140360.
14. Gwini S, Macfarlane E, Del Monaco A, et al. Cancer incidence, mortality, and blood lead levels among workers exposed to inorganic lead. Ann Epidemiol. 2012;22(4):270-276. doi:10.1016/j.annepidem.2012.01.003.
15. Gervasio A. Lamas, MD; Christine Goertz, DC, PhD; Robin Boineau, MD, MA; et alDaniel B. Mark, MD, MPH; Theodore Rozema, MD; Richard L. Nahin, PhD, MPH; Lauren Lindblad, MS; Eldrin F. Lewis, MD, MPH; Jeanne Drisko, MD; Kerry L. Lee, PhD; for the TACT Investigators Effect of Disodium EDTA Chelation Regimen on Cardiovascular Events in Patients With Previous Myocardial Infarction The TACT Randomized Trial, JAMA. 2013;309(12):1241-1250. doi:10.1001/jama.2013.2107
16.Ja-Liang Lin, M.D.,Dan-Tzu Lin-Tan, R.N., Kuang-Hung Hsu, Ph.D., and Chun-Chen Yu, M.D, Environmental Lead Exposure and Progression of Chronic Renal Diseases in Patients without Diabetes, N Engl J Med 2003; 348:277-286 DOI: 10.1056/NEJMoa021672
Disclaimer:
This blog provides general information and discussions about health and related subjects. The information and other content provided in this blog, website or in any linked materials are not intended and should not be considered, or used as a substitute for, medical advice, diagnosis or treatment. This blog does not constitute the practice of any medical, nursing or other professional health care advice, diagnosis or treatment. We cannot diagnose conditions, provide second opinions or make specific treatment recommendations through this blog or website.
If you or any other person has a medical concern, you should consult with your health care provider or seek other professional medical treatment immediately. Never disregard professional medical advice or delay in seeking it because of something that you have read on this blog, website or in any linked materials. If you are experiencing a medical emergency, please call 911 or call for emergency medical help on the nearest telephone immediately.

